The theory that 'gut bacteria cause autism' may be wrong

In recent years,
Autism-related dietary preferences mediate autism-gut microbiome associations: Cell
https://www.cell.com/cell/fulltext/S0092-8674 (21) 01231-9
Gut bacteria don't cause autism. Autistic kids' microbiome differences are due to picky eating
https://theconversation.com/gut-bacteria-dont-cause-autism-autistic-kids-microbiome-differences-are-due-to-picky-eating-170366
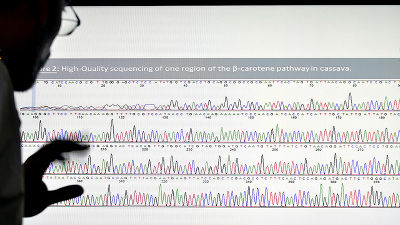
From the observations that 'people with autism spectrum disorders (ASD) , including developmental disorders such as autism, Asperger's syndrome, and pervasive developmental disorders, are more likely to experience intestinal problems such as constipation and diarrhea,' the intestines. Attention is focused on the relationship between the internal flora and autism. So far, research results have shown that 'giving mice the intestinal flora of people with ASD behaves like autism' and 'therapy using the intestinal flora alleviates the symptoms of autism. of that ' research result , further' people of children and non-ASD of ASD is there is a difference in the intestinal flora 'that the research results have been such reports.
From these findings, some researchers argue that the gut microbiota causes autism, but Dr. Chloe Yap and colleagues at the University of Queensland say, 'This excitement is It's misguided. ' Comparing the results of all studies, the evidence linking the gut microbiota to autism is inconsistent, and many studies have serious scientific design problems .
However, despite scientific uncertainties, the hype linking autism to the gut microbiota is gaining momentum, with unfounded 'gut microbiota therapy' and 'gut microbiota' claiming to treat autism. 'Diet therapy' is also appearing. Dr. Yap and colleagues point out that these treatments are not effective and safe, and can have adverse health effects.

The study collected fecal samples from 99 children with ASD, 51 children with autistic siblings but not autistic, and 97 children without autistic siblings. For fecal samples, we compared the DNA of the microorganisms contained in the samples. He also investigated a wide range of factors that affect the intestinal flora, such as child clinical data, family structure, lifestyle, and diet.
Analysis revealed no association between autism and the composition or diversity of the entire gut flora, and only one of the more than 600 gut bacteria was associated with autism. Only found. The research team points out that no association with autism was found in this study for multiple bacterial groups that were previously associated with autism.
Instead, it was also confirmed that children with ASD are more likely to 'have a lot of likes and dislikes of food,' as
In addition, an analysis that took genetic data into account showed that autism and limited interests were associated with an unbalanced diet, but did not directly correspond to the gut flora. 'Overall, our findings did not support the general view that the gut microbiota causes autism. What we propose instead is surprisingly simple. Autism. Disease-related traits and preferences are associated with a less diverse diet, which results in a less diverse gut flora and diarrheal stools, 'says Dr. Yap and colleagues.
The findings suggest that interventions such as gut microbiota transplantation for people with autism should be cautious. He argued that eating habits should be supported for children with autism who are prone to unbalanced diets, rather than being interested in potentially harmful treatments.

Related Posts:
in Science, Posted by log1h_ik