Finally succeeded in testing cancer treatment with gene editing technology `` CRISPR '', attacking tumors by custom-made genome-edited immune cells

Researchers have announced that they have successfully tested to accurately attack cancer malignant tumors by creating 'genome-edited immune cells' for each individual using the gene-editing technology '
CRISPR cancer trial success paves the way for personalized treatments
https://www.nature.com/articles/d41586-022-03676-7
The study published this time is the first attempt to successfully combine two hot fields of cancer research, notes the journal Nature . Two hot areas are creating personalized therapies through gene editing and targeting tumors by manipulating immune cells called T cells .
In the study, cancer treatment using CRISPR is performed on 16 cancer patients with solid tumors , including breast and colon.
'This is probably the most complex treatment ever attempted in the clinic,' said study co-author Antoni Rivas, a cancer researcher and physician at the University of California, Los Angeles. I'm trying to create an army that destroys cancer tumors from my own T cells.'
Rivas and his team have sequenced DNA from blood samples and tumor
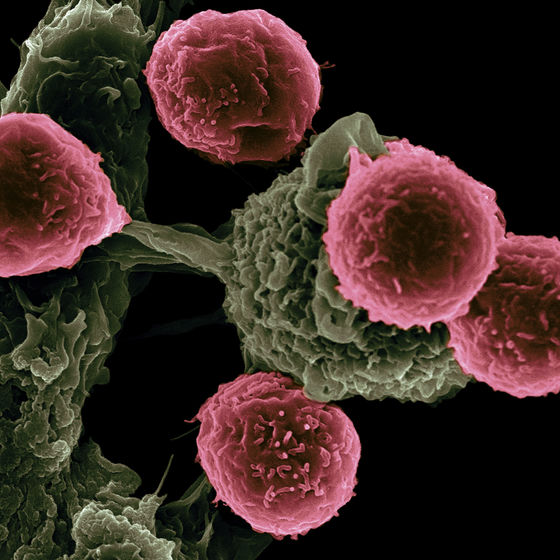
After identifying mutant proteins, the researchers used algorithms to predict which mutations are likely to trigger a response from T cells. 'When T cells find something wrong, they destroy it. But in the cancer patients we see in the clinic, at some point the immune system loses the battle and the tumor grows.' said Stephanie Mandle, chief scientific officer at PACT Pharma in South San Francisco, Calif., and lead author of the study.
After validating the algorithm's predictions, the research team conducted an analysis to design proteins called T-cell receptors that can recognize mutations in tumors. Then, take a blood sample from the subject and use CRISPR to insert the receptor into the T cell. Each subject was then injected with CRISPR-generated T cells after taking a drug to reduce the number of immune cells produced.
``This is a tremendously complex manufacturing process,'' said Joseph Flatta of the University of Pennsylvania, who studies cancer treatments using T cells. According to the research team, in some cases it may take more than a year for the `` process of customizing T cells for individuals with CRISPR ''.
Sixteen subjects in the study were infused with T cells that were gene-edited to have up to three different targets. After that, it was confirmed that gene-edited T cells circulated in the blood, and it was also confirmed that they were present in higher concentrations near the tumor than non-gene-edited T cells. After one month of this treatment process, five of the subjects were also confirmed to have transitioned to a stable condition. In other words, it was confirmed that the tumor had not grown. Two out of 16 people have experienced side effects that are likely due to 'gene-edited T cells'.
Although treatment efficacy was low, they were successful in using relatively small amounts of T cells to establish the safety of the approach, Rivas said. Also, as the research team develops methods to accelerate the development of therapeutics, gene-edited cells will spend less time in vitro and become more active when injected. Mr. Flatta also said, 'Technology will gradually improve.'
Treatments using genetically engineered T cells are called CAR-T cell therapy . CAR-T cell therapy has been approved for use in the treatment of some hematological and lymphatic cancers, but has proven difficult to apply to solid tumors. This is because CAR-T cells are only effective against proteins expressed on the surface of tumor cells. Because this type of protein is common to many hematological and lymphatic cancers, there was no need to design new T-cell receptors for these cancer patients.
However, no common surface protein is found in solid tumors from patient to patient. Therefore, therapy using CAR-T cells was not effective against solid tumors. T cells must also circulate in the blood, travel to tumors, infiltrate, and destroy cancer cells. However, tumor cells may release chemical signals that suppress immunity and suppress immune responses. ``The environment around the tumor is like a sewer,'' Flatta said.
The research team hopes to use CAR-T cells not only to recognize cancer mutations, but also to make T cells more active near the tumor. There are several ways to strengthen T cells, Mandl said, including 'removing receptors that respond to immunosuppressive signals' and 'making it easier for them to find energy sources in the tumor environment.' 'Adjust your metabolism.'
'CAR-T cell technology has become incredibly efficient,' said Avery Posei, who studies gene therapy for cancer treatment at the University of Pennsylvania. There will be very sophisticated methods of genetic manipulation,' he said.
Related Posts:
in Science, Posted by logu_ii