World's first achievement: iPS cell transplant enables type 1 diabetes patients to produce insulin
A research team from Peking University announced that they had succeeded in treating a patient by creating insulin-synthesizing cells from patient-derived iPS cells and transplanting them into the patient, achieving almost complete blood sugar control without the need for insulin administration.
Transplantation of chemically induced pluripotent stem-cell-derived islets under abdominal anterior rectus sheath in a type 1 diabetes patient: Cell
Stem cells reverse woman's diabetes — a world first
https://www.nature.com/articles/d41586-024-03129-3
It is said that there are 500 million people with diabetes in the world. Most of them have type 2 diabetes, but some have type 1 diabetes, in which the immune system attacks the islet cells in the pancreas that produce insulin, resulting in little or no insulin secretion.
To treat type 1 diabetes, islet transplants are performed in which islets are extracted from a donor's pancreas and transplanted into the patient's liver. However, immunosuppressants are required to prevent the patient's body from rejecting the donor's cells.
On the other hand, stem cells can be used to grow any tissue from the body in the laboratory, potentially providing an unlimited source of islet transplants, and using a patient's own cells would eliminate the need for immunosuppressants.

Now, cell biologist Deng Hongkui of Peking University and his team have taken cells from three patients with type 1 diabetes and returned them to a pluripotent state, allowing them to differentiate into any cell type.
This reprogramming technology was developed in 2006 by Shinya Yamanaka of Kyoto University in the form of iPS cells, but genetic reprogramming carries the risk of unexpected mutations and cancer.
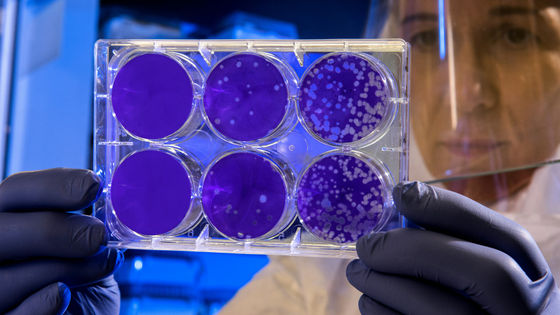
This time, the team used CiPS cell technology, previously developed by other researchers, to create clusters of pancreatic islet cells from the patient's cells, using more precise control of the differentiation process using only chemicals.
In the transplant surgery in June 2023, about 1.5 million islets were transplanted into the liver of a female patient in just 30 minutes, and two and a half months later, the woman was able to secrete enough insulin to live without insulin supplementation. The reason why the islets are transplanted into the liver rather than the pancreas is because
Treated women have maintained high insulin levels for over a year and achieve blood sugar levels within target range 98% of the time, without dangerous swings in blood sugar.
'This is amazing,' Daisuke Yabe, a diabetes researcher at Kyoto University, told the scientific journal Nature. 'It would be fantastic if this could be applied to other patients.'
Jay Skyler, a type 1 diabetes researcher at the University of Miami in Florida, said the woman's cells would need to continue producing insulin for up to five years before they could be considered 'cured.'
'In addition, because the women had already been given immunosuppressants from previous transplants, the risk of rejection could not be assessed in this study. In addition, because most cases of type 1 diabetes are caused by autoimmune factors, even if the transplanted cells were not rejected by the body as 'foreign,' there is still a risk that the immune system would attack the islets.'
Deng said the progress of the other two type 1 diabetes patients is 'very positive' and will reach the one-year milestone of treatment in November 2024. The team plans to expand the study to 10 to 20 people in the future.
Other promising results have been reported from stem cell-based diabetes treatments, such as a study led by Vertex Pharmaceuticals, a biopharmaceutical company in Boston, Massachusetts, in which 12 participants with type 1 diabetes were given stem cell-derived pancreatic islets transplanted into their livers while receiving immunosuppressants. All participants were able to secrete insulin, although some no longer needed insulin.
Yabe has also begun preparations for tests on pancreatic islet cells created from donor iPS cells, and a transplant surgery using the islet cell sheet he developed is scheduled to take place in February 2025.
Kyoto University Hospital submits clinical trial plan to use iPS cells for diabetes treatment to government | NHK Kyoto Prefecture News

Related Posts:
in Science, Posted by log1l_ks