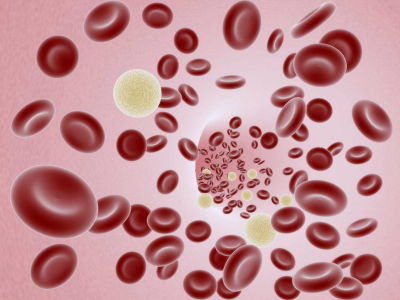
How far have artificial red blood cells become a reality?

Because transfused blood has a short shelf life, even developed countries with a well-established blood donation system suffer from chronic blood shortages. The American scientific journal Science has summarized the current status and future of artificial blood, which is expected to solve this problem.
The ultimate blood substitute? The US military is betting $46 million on it | Science | AAAS
One of the technologies that has attracted the most attention as a blood substitute is ' Erythromer ,' which is made from human hemoglobin. Erythromer can be stored in powder form for long periods of time and can be used simply by mixing it with saline when needed. Since it does not contain the substance on the surface of red blood cells that causes blood type incompatibility, it can be used for any blood type.
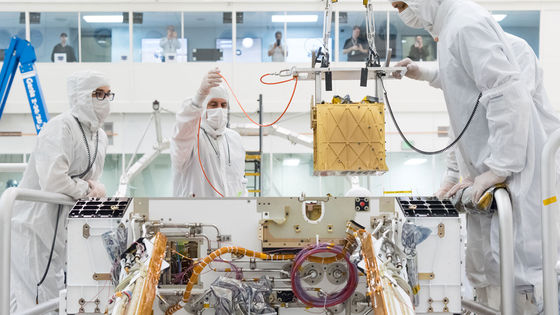
Erythromycin is still in the research stage prior to clinical trials and has not yet been shown to be a clinical success. However, efforts toward its practical application are gaining momentum, such as the announcement by the U.S. Defense Advanced Research Projects Agency (DARPA) that it will invest $46 million (approximately 7.3 billion yen) in 2023 to research whole blood substitutes containing erythromycin.

However, Erythromycin's success is not guaranteed. Its predecessor, hemoglobin-based oxygen carriers (HBOCs), have stalled research after previous clinical trials led to deaths. The most advanced HBOCs approved in South Africa and Russia so far also face difficult times due to persistent concerns about side effects.
The difficulty in developing artificial blood lies in the technology to safely replicate the functions of hemoglobin. Firstly, hemoglobin itself is a difficult molecule to handle, and if used as is in blood, it would be harmful to blood vessels and body tissues. In addition, the oxygen it carries acts as an oxidant that is harmful to the human body, and if oxygen is released at the wrong time or in the wrong place, it could have devastating effects.
In addition to oxygen, nitric oxide is also a problem. When red blood cells deliver oxygen to active muscles, they also release nitric oxide, which dilates blood vessels and increases blood flow. When exercise ends, red blood cells stop releasing large amounts of oxygen, but at this time nitric oxide binds to hemoglobin and is absorbed, causing blood vessels to constrict.
Unable to adequately replicate the effects of red blood cells, HBOCs use unprotected hemoglobin, which can lead to excessive uptake of nitric oxide, which can cause blood vessels to constrict, potentially leading to heart attacks and strokes.
On the other hand, the hemoglobin in Erythromycin, developed by Alan Doctor and his colleagues at the University of Maryland, is surrounded by a membrane, which means that it absorbs nitric oxide only slowly.
Erythromycin has been shown to have some success in animal testing, and when 70% of a mouse's blood was replaced with erythromycin, it was shown to effectively supply oxygen. In addition, when half of a rabbit's blood was removed, it was confirmed that the rabbit was resuscitated by injecting erythromycin just as if it had been given real blood.
Doctor and his team hope to conduct initial safety trials of erythromycin in healthy humans around 2028, when the DARPA grant ends.
'We don't have enough Rh-negative blood to provide for everyone,' he told Science. 'We need blood that can be stored and used by everyone.'
Related Posts:
in Science, Posted by log1l_ks