It turned out that the brain of a woman diagnosed with severe schizophrenia was damaged by an autoimmune disease, so that she could talk to her family for the first time in 20 years after receiving treatment

In the past, many people thought that mental illness was a “mental or emotional problem,” but in recent years, mental illness is closely related to various physical problems, and it is often said that mental illness is caused by physical causes. We know that there are cases where A woman who was diagnosed with severe
How autoimmune disease can attack the brain, cause psychiatric symptoms - The Washington Post
https://www.washingtonpost.com/wellness/2023/06/01/schizophrenia-autoimmune-lupus-psychiatry/

April Burrell, who grew up in Baltimore, Maryland, USA, devoted herself to volleyball and studying when she was in high school, and was an excellent student who served as the valedictorian of her high school. Although I majored in accounting in college and showed no signs of mental illness, a traumatic event in 1995 landed me in a mental hospital. To protect privacy, the Washington Post did not describe what happened specifically.
In addition to being diagnosed with severe schizophrenia, Mr. Burrell is also a severe catatonia that stops moving with abnormal behavior and strange postures, and is so serious that he needs assistance in bathing and daily life. In 2000, he moved to the Pilgrim Psychiatric Center in New York State for long-term care. While the family made monthly trips to the Pilgrim Psychiatric Center, a four-hour trip each way, Mr. Burrell shut himself away in his own world, fingering what looked like formulas and muttering to himself about financial transactions. He just couldn't communicate.
In 2000, when Burrell moved to the Pilgrim Psychiatric Center, Sander Marks, who was still a medical student at the time, visited the Pilgrim Psychiatric Center as a scholarship student from the Netherlands. There, Mr. Marks said he saw Mr. Burrell, who was particularly severe among hospitalized patients.
'She was just standing at the nurses station,' Marks recalled. I had to.' 'She was the sickest patient I've ever seen.'

Marks went on to become a researcher and in 2018 became the director of precision psychiatry at Columbia University and has his own laboratory. Meanwhile, when a trainee visited the Pilgrim Psychiatric Center at Mr. Marks' suggestion, he told Mr. Marks an episode that ``I witnessed a catatonic patient standing by a nurse's desk.'' Mr. Marks, who heard the story, recalled about 20 years ago, ``I felt deja vu when he started talking, and asked, 'Is her name April?' said.
In fact, the woman who the trainee witnessed was Mr. Burrell, and Mr. Marks was astonished when he learned that his medical condition had hardly changed for 20 years. Even after Mr. Marks first met Mr. Burrell, doctors continued to administer antipsychotics, tranquilizers, and electroconvulsive therapy, but all to no avail.
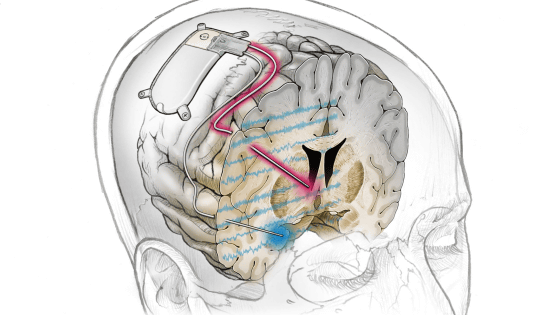
With the consent of Mr. Burrell's family, Mr. Marks and others convened an interdisciplinary team of more than 70 experts from around the world to conduct a thorough investigation of what was happening to Mr. Burrell's body. Did. Blood tests revealed that Burrell's immune system was producing large amounts of antibodies that attacked his own body, and that these antibodies attacked the temporal lobe of the brain associated with schizophrenia. Did.
Mr. Burrell certainly showed clinical symptoms of schizophrenia, but the cause was

After several months of cycles, including intravenous steroid injections, intensive administration of
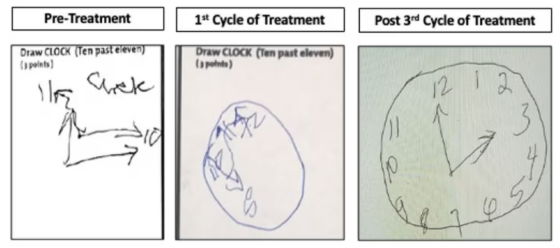
The image below is the result of Mr. Burrell doing the task 'drawing a clock' as part of the cognitive test. The leftmost picture is before treatment, and although you can barely see the hands of the clock and the numbers '11' and '10', it is not at a level that can be distinguished as a clock. However, when you look at the middle picture after completing one cycle, you can see something that looks like a number and something that looks like a clock hand in a circle, and if you look at the picture on the far right after completing three cycles, you can see a clock. I'm recovering to a level that I can clearly understand.
Still, Mr. Barrell continued to have symptoms of mental illness, but he said that he had recovered so much that he was no longer comparable to before treatment. In 2020, he was discharged from the Pilgrim Psychiatric Center and moved to a rehabilitation center, and in 2022, when visitation restrictions due to the new coronavirus infection (COVID-19) were lifted, Mr. Burrell was finally able to meet his family. .
Although not fully recovered, Burrell's family said he remembers his past, including memories of his childhood and attending his brother's wedding. In addition, Mr. Burrell was able to recognize that he had grown up and became an adult because he was still a child before the onset. He could have even said and laughed.
'She was hugging me and holding my hand,' said brother Guy Burrell. 'It was like she was coming home. We never thought it was possible. I didn't,' he said.

After Mr. Barrell recovered, the research team expanded the scope of the investigation to see if there were other patients with autoimmune diseases. As a result, it turned out that a woman named Divine Cruz, who was diagnosed with schizophrenia at the age of 9, was diagnosed with systemic lupus erythematosus at the age of 14. However, autoimmune diseases were never associated with schizophrenia, and it was difficult to live a daily life as of 2022 when I was 20 years old.
When the research team started treatment with steroids and immunosuppressants in the same way as Mr. Barrell from August 2022, the symptoms dramatically improved in October, just two months later. Mr. Cruz was suffering from auditory hallucinations and various hallucinations in which he heard multiple voices in his brain, but gradually he was able to recognize that ``the voices in his head are not real'', and in January 2023 I have completed my treatment cycle. In March, he was able to respond to an interview with a Washington Post reporter, and was able to talk about the symptoms he was experiencing as a child and the delusions that often hit him.
At the time of writing the article, Mr. Cruise's auditory hallucinations and hallucinations have subsided, and he no longer meets the criteria for schizophrenia. Cruz lives with her mother and has recovered enough to help cook, shop, ride public transportation and care for her young siblings. 'Without their help, I wouldn't be here,' Cruz said. 'It feels like a new chapter in my life and I'm thrilled. I commented.
Following the cases of Mr. Burrell and Mr. Cruz, Columbia University used a $ 75 million (about 10.4 billion yen) grant from the international charity
The SNF Center for Precision Psychiatry and Mental Health is also partnering with the New York State Department of Health and Mental Health to screen long-term hospitalized psychiatric patients to find those with autoimmune causes. About 40 patients have already started treatment based on the autoimmune disease approach, and they plan to expand the screening test to outpatients in the future.

Related Posts:
in Science, Posted by log1h_ik