Survival with cardiopulmonary resuscitation (CPR) is lower than expected
'
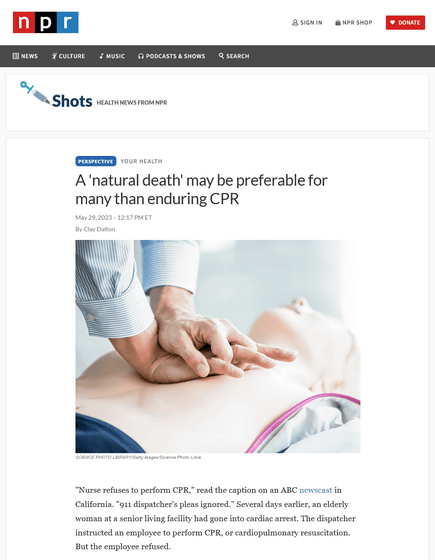
CPR's true survival rate is lower than many people think : Shots - Health News : NPR
https://www.npr.org/sections/health-shots/2023/05/29/1177914622/a-natural-death-may-be-preferable-for-many-than-enduring-cpr
In 1878, an experiment with cats revealed that the blood can be circulated by compressing the sternum during cardiac arrest.
About 80 years later, in 1959,
However, CPR is by no means a “just do it and you will be saved” treatment.
According to the 2015 paper ' It isn't like this on TV: Revisiting CPR survival rates depicted on popular TV shows': A survey of the 2010-2011 broadcasts of the medical dramas `` Grey's Anatomy '' and `` Doctor House '' found that 46 episodes of cardiopulmonary resuscitation were depicted in 91 episodes, and the survival rate was 69.6%. . 71.9% of patients were resuscitated immediately after CPR and the majority were discharged without incident, and 15.6% died before discharge. There were only two depictions of arguments about advance directives. The research team said that the survival rate is depicted in the drama higher than it actually is, ``This inaccurate depiction can mislead viewers and affect critical illness and end-of-life care decisions.'' concludes.
Also in a 2015 paper, ' What CPR means to surrogate decision makers of ICU patients ,' 72% of 97 subjects had a CPR survival rate of 75%. It has been pointed out that they believed that it was more than that.
In fact, a 2010 paper examining 79 studies of about 150,000 out-of-hospital cardiac arrest patients found that the survival rate for out-of-hospital cardiac arrest remained unchanged for nearly 30 years at 7.6. %. And it has been shown that the survival rate when a third party performed CPR was 10%, and the CPR survival rate when cardiac arrest occurred in the hospital was 17%.

As the patient ages, the value of the CPR survival rate decreases, and in a Swedish study, the CPR survival rate during out-of-hospital cardiac arrest was 6.7% for patients in their 70s and 2.4% for patients in their 90s. Chronic disease also affects survival, with less than 2% of cancer patients and patients with heart, lung, and liver disease surviving six months after CPR.
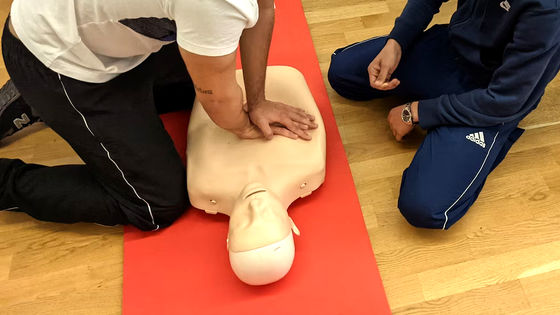
Dalton pointed out that compressing the sternum itself is harmful to the body in the first place, in response to the idea that ``if there is even a slight possibility of resuscitation, it will be a motivation to try CPR.'' When researchers at Johns Hopkins University first performed CPR, ``complications include rib fractures and cracks,'' as well as pulmonary hemorrhage and liver laceration.
Especially in the elderly, the wounds inflicted by CPR are often irreversible, and one study found that 38.6% of patients over the age of 70 who survived CPR recovered their function. .
In addition, there are cases in which the brain and other organs are damaged while the heart stops temporarily, and about 30% of patients who survive CPR in cases of in-hospital cardiac arrest
In addition, Dalton points out that CPR can affect not only patients but also healthcare workers.
As an example, Dr. Holland Kaplan, a doctor and bioethicist, has posted on the university's official blog what he experienced during his residency at Baylor College of Medicine.
Code blues: When is CPR not useful? - Baylor College of Medicine Blog Network
https://blogs.bcm.edu/2019/02/22/code-blues-when-is-cpr-not-useful/
Kaplan performed CPR on an 82-year-old man with end-stage heart failure and metastatic cancer who did not want blood products for intestinal bleeding. Even before performing CPR, Mr. Kaplan seems to have understood that this was a 'show code', that is, 'an effort to resuscitate a patient who knows that this procedure is useless.'
When performing CPR, Kaplan recalled being told that the ribs didn't break because he wasn't doing the chest compressions correctly. I look back on the senses as 'the most sickening experience in my medical training.'
Ultimately, the man's family agreed that further resuscitation measures were futile, and the man died. Emergency response to cardiac arrest patients is called 'code blue', but Mr. Kaplan said that he became afraid of 'code blue'.
However, even with these problems, it is difficult to argue that CPR should not be performed . As of 2017 , bioethicists Philip Rosoff and Lawrence Schneiderman states that 'CPR has acquired an almost mythical reputation and atmosphere,' and that 'not doing CPR may look like not throwing a rope at a drowning man.' increase.
Related Posts:
in Science, Posted by logc_nt