Why did the 'WHO Checklist', which should drastically reduce medical errors during surgery, not work well in the field?

by
In 2008, the World Health Organization (WHO) published a “ surgical safety checklist ” with the touch of halving the mortality rate from surgery, and urged hospitals around the world to implement it. However, subsequent fact-finding surveys have found cases where medical errors and accidents have hardly decreased even when checklists are used. Or check list that would save the life of the patient is the integral what the reason was hardly function in some cases, the journalist Emily Ansesu Mr., follow the cause from the survey results to the medical practice of the actual situation and doctors It was.
Hospital checklists are meant to save lives — so why do they often fail ?: Nature News & Comment
https://www.nature.com/news/hospital-checklists-are-meant-to-save-lives-so-why-do-they-often-fail-1.18057
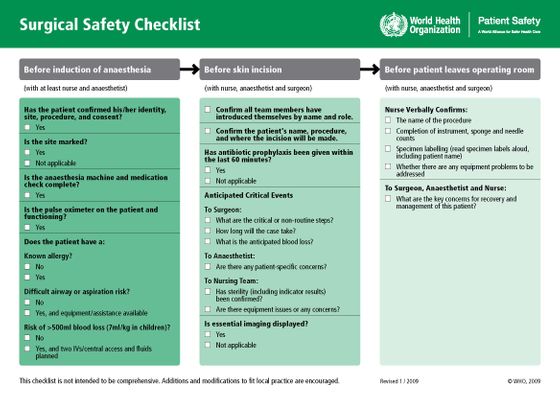
The “surgical safety checklist” created by WHO contains 19 questions such as “Is there any known allergies for patients?” Or “Is there a risk of blood loss exceeding 500 ml?” It covers everything from previous confirmation items to post-operative inspections. Prior to the announcement, eight hospitals piloted the checklist, reducing the risk of complications such as postoperative infections by one-third and reducing mortality by almost half. Encourage medical institutions around the world to implement a checklist or similar system. By 2012, more than 2000 medical institutions around the world followed it.
The following image is a revised version of the surgical safety checklist actually created by WHO.
However, research results that raise questions about the effectiveness of the checklist have since been published. For example,
◆ Indication that checklist is not effective in the first place
Some researchers have pointed out that this discrepancy is “there was a flaw in the first demonstration test in the first place”. In the research report of Atul Gwande, a researcher who led the WHO trial and a doctor at the Brigham and Women's Hospital in Boston, the empirical trial was not randomized and compared to the control group. We simply compared the number of complications and deaths before and after the introduction of the checklist. This means that factors other than the checklist, such as advances in medical technology and device updates, are not excluded from the survey results.
However, Mr. Gawande, who became a best-selling writer in the non-fiction novel “ The Checklist Manifesto ” related to the checklist, admits that his investigation was costly constrained. It is argued that its usefulness has been fully demonstrated. “The checklist works properly, as long as it works properly,” he said.
◆ Possibility of problems in operation
In fact, research results supporting Gwande's objection have been reported. The UK medical institution required the introduction of a WHO checklist by the state-run medical service business , and the research team of Nick Sevdalis and colleagues at Imperial College London followed up to check the status of the checklist in practice. We conducted a survey .

by
As a result, 96.7% of 6714 surgeries used checklists, but only 62.1% completed the list to the end. In more than 40% of cases, some of the surgical staff did not participate in the check, and in 10%, the check was performed without the chief surgeon. In addition, the study found that the more items checked, the lower the incidence of postoperative complications.
Sevdalis and colleagues interviewed more than 100 surgical staff working at medical institutions in the UK to find out why the checklist was not operating properly. As a result, half of the respondents answered that “upper surgeons and anesthesiologists are extremely uncooperative with the checklist”, and one-quarter of the staff are also dissatisfied with how the checklist was introduced. It was. This is because only a few medical institutions trained or solicited opinions from the staff when introducing checklists, and most medical institutions required the use of checklists, regardless of whether they were present or not.
Also, Mary Dixon-Woods, a medical sociologist at the University of Leicester, interviewed both a British medical professional and a Boston medical professional who participated in the WHO trial. I have been engaged in various initiatives led by me, and the fact that I was exhausted has emerged. In contrast, the WHO checklist was seen as “one of the top-down push-in measures,” but in contrast, Boston medical staff clarified the checklist as “new and groundbreaking. It was said that it was a 'simple approach', and he was looking for participation in the verification test.

by FlamingoImages
◆ Medical environment issues
Even when the checklist was introduced, there were cases where the medical environment was poorly organized. When Dickson-Woods surveyed African hospitals adopting the WHO checklist, they found that they tend to run out of surgical skin markers, antibiotics, pulse oximeters, etc. as listed. I understand.
From this, Mr. Dixon-Woods said, “Although it was better for the patient to perform surgery even if it was not a perfect system, there was no antibiotic, but the check item“ Did you administer antibiotics? ” It ’s not effective even if it ’s marked. ”
Ances said, “A clear lesson for medical institution managers is that it is meaningless to just throw a check sheet into the operating room,” and not just pushing the checklist against the medical staff, I indicated that I need to look closely.
Related Posts:
in Note, Posted by log1l_ks







