Why did the new Corona stop its rapid spread before it could infect 80% of the population?

The new coronavirus infectious disease (COVID-19) was prevalent in many countries around the world, and medical pressure was a problem at one point, but the spread of infection is gradually turning to a convergence trend in the United States, Europe, and Japan. The situation is still uncertain, and the reason why the rapid spread of infection has stopped is not clear, but from the results of the research so far, 'a possibility that humans have acquired immunity other than antibodies' was started as a software engineer. House's
COVID-19: The T Cell Story-Articles
https://berthub.eu/articles/posts/covid-19-t-cells/
When the COVID-19 epidemic began, it was thought that 'antibody against the new coronavirus (SARS-CoV-2) does not exist in the human body beforehand, and there is a possibility that all people will be infected with the virus.' For this reason, it was deduced that 80% of the population could be infected with the virus before they acquired collective immunity.
However, even months after the pandemic, 80% of the population has not been infected.
◆Why did the spread of COVID-19 infection level off early?
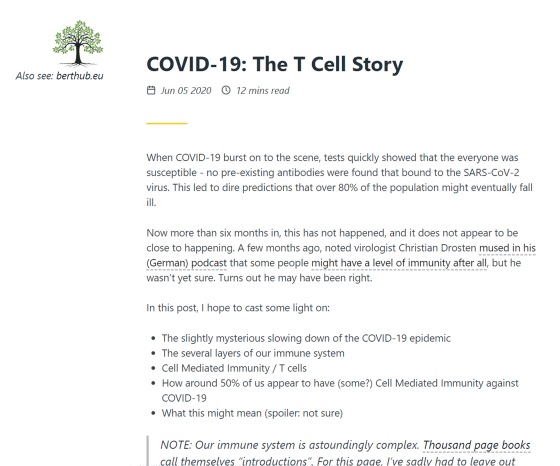
Although SARS-CoV-2 is still a mystery, several possibilities have emerged from the above background. First, while some countries have undergone large-scale COVID-19 testing, others have not taken a dramatic strategy, but in all countries the infection rate exceeds 10-20% of the population. Previously, the graph showing the number of infected people has leveled off. 'This is a strange phenomenon,' Herbert said.
From various research results, it is thought that COVID-19 will infect 2-3 people from one infected person, and the spread of infection will occur 'rapidly' until 60% of the population is infected with the virus. I came. However, actual research has shown that many people, whether they live together or sleep in the same bed, do not transmit the virus to others.
This phenomenon is called 'overdispersion.' In other words, although it is said that “on average, one to two to three people will be infected”, there is uneven distribution, and there are “a large number of people who rarely get infected” and “a small number of people who get many people infected”. It is conceivable that 'people of' exist.
Taking into account overdispersion due to different susceptibility to human infections, it could also explain that the rate of spread is flat before 60% of the population is infected, Herbert said. Simply put, if 15% of the population can be easily infected with a virus, once the infection rate reaches 15%, the virus will be difficult to spread.
Of course, some scientists argue that this idea is 'problematic,' so the reality is still unknown. On the other hand, based on the above hypothesis, Mr. Harvard is examining 'why some people are less likely to have COVID-19 and some people are more likely to have COVID-19' from the mechanism of human immune function.
◆Immune system consists of multiple layers

'Antibodies' that can be examined by antibody tests are one of the human immune functions, but the human body has various immune functions in addition to viral antibodies. These include the presence of 'mucus' that prevents viruses from contacting cells, and the 'natural immune system' that attacks unknown pathogens.
At low exposure to viruses, so-called 'early stage' immune systems, such as mucus, can prevent infection. If the virus cannot enter the body without being protected by such an immune system, the antibody produced in the body recognizes and binds to the virus, which is the stage of killing the virus in the body.
However, antibodies are important for effectively disabling the virus, but it is not a perfect solution in the body where trillions of viruses are continuously copied. In such cases, cell-mediated immunity, which kills the cells that are infected with the virus and continue to replicate DNA, plays a major role.
Cellular immunity means that immune cells themselves such as T cells attack abnormal cells such as virus-infected cells and cancer cells without passing through antibodies. In order to identify cells infected with virus by immune cells, use the mark whether or not peptides obtained from viral proteins appear on glycoprotein/ MHC on the surface of cells.
Antibody testing can be performed relatively easily and quickly. For this reason, antibody tests have already been carried out in various countries, but at the time of writing the article, a certain population did not show a high antibody prevalence rate.
On the other hand, it is extremely difficult to test whether cell-mediated immunity is functioning. Cellular immunity testing is not realistic because it requires the expression of a fragment of SARS-CoV-2 on the MHC molecule on the cell surface to test whether T cells respond to it. For this reason, it is not yet clear whether people are protecting their bodies from SARS-CoV-2 through cell-mediated immunity.
However, some studies have reported good response of T and B cells to SARS-CoV-2.
What kind of cells are 'T cells' that are the key to the possibility of acquiring immunity to the new coronavirus? -GIGAZINE

Although it cannot be said from the results of the test that “many people already have antibodies against SARS-CoV-2”, from the study of T cells and B cells, more people than expected to SARS-CoV-2. It is possible that you have immunity. On the other hand, there are some signs that COVID-19 is better at evading the cellular immune response.
Although these possibilities were unproven at the time of writing, Herbert said the subject will be intensively researched in the coming months.
Related Posts:
in Science, Posted by darkhorse_log