Succeeded in culturing human 'mini lungs', finding a way to study pandemics like the new corona
Organotypic human lung bud microarrays identify BMP-dependent SARS-CoV-2 infection in lung cells: Stem Cell Reports
https://doi.org/10.1016/j.stemcr.2023.03.015
Lab-Grown Mini Lungs: Accelerating Respiratory Disease Research
https://scitechdaily.com/lab-grown-mini-lungs-accelerating-respiratory-disease-research/
The new coronavirus infection (COVID-19), which was called a once-in-a-century pandemic, has been raging with more than 665 million infected people and more than 6.7 million victims so far. . In order to deal with the explosive spread of COVID-19, it is essential to study how the pathogen, the new coronavirus (SARS-CoV-2), infects the human lungs. I have a difficult task.
Because the properties of lung tissue vary from person to person, the mechanism by which SARS-CoV-2 first infects lung cells has not been elucidated. Current COVID-19 research relies on experiments with primary human lung tissue, lung cells donated directly from a living person, but the lung cells produced in this way are genetic. It is not possible to obtain uniform and highly accurate data because the
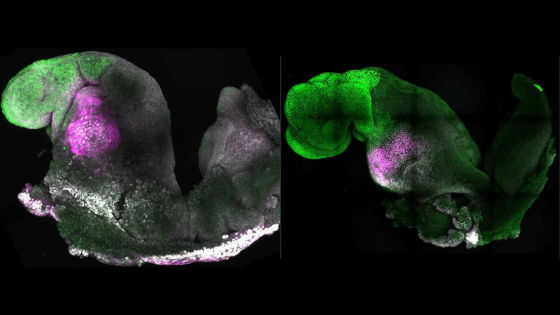
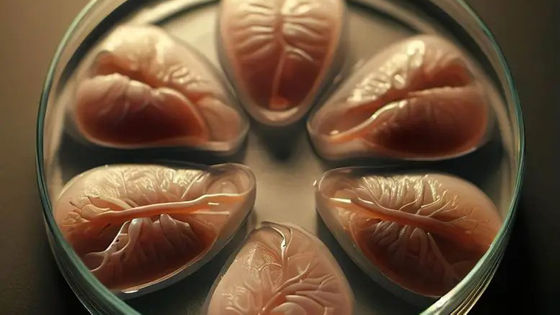
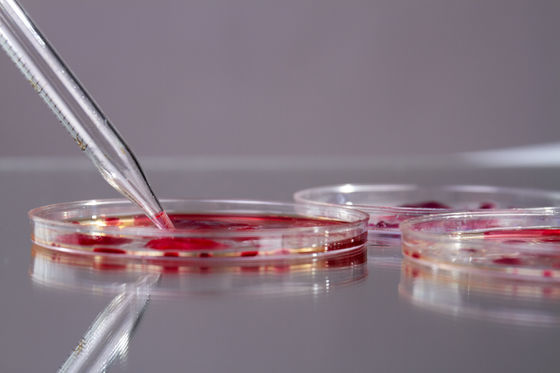
Therefore, a research team led by Ari Brivanloo and Charles M. Rice of the Rockefeller University placed human ES cells on a microchip and placed lung buds (the original tissue of the respiratory tract) with the same genes. ) has been developed. Thousands of these lung buds can be cultured in large quantities, and since there are no genetic differences, it is possible to collect uniform and large-scale infection data.
'These lungs are basically clones, so there's no worry that one patient will react differently to another,' said Brivanloo.
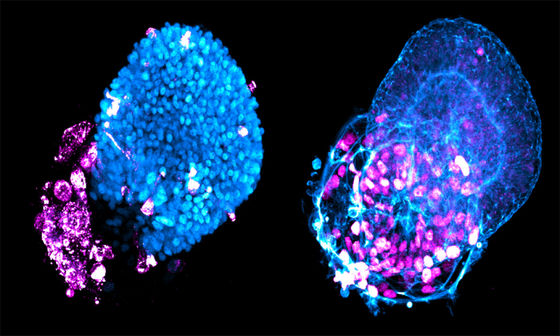
Brivanloo, who has been researching technology to grow lung buds on microchips for many years, and Rice's lab, which has the biosafety level necessary for experiments to infect SARS-CoV-2, have collaborated to grow cultured mini-lungs into viruses. In an experiment, it was found that alveoli are more susceptible to infection than airway cells. Airway cells, which are the passageway of air to the lungs, have the role of a protective wall that protects the alveoli that exchange gas during respiration, but if SARS-CoV-2 slips through the airway cells, the alveoli is a good duck.
Below is a picture of the alveoli (left) and airway cells (right) of the mini-lung created by the research team being infected with SARS-CoV-2. Cells are in blue, and viruses are in purple.
According to the research team, the technology developed this time can be used not only for COVID-19 but also for elucidating the mechanisms of influenza, other respiratory infections, lung diseases, lung cancer, etc. Screening of new drugs used for their treatment It can also be used for
“This platform will also enable us to respond more quickly and accurately to the next pandemic,” Brivanloo said. We will be able to develop a treatment for this,' he said.
Related Posts:
in Science, Posted by log1l_ks